Gastric band
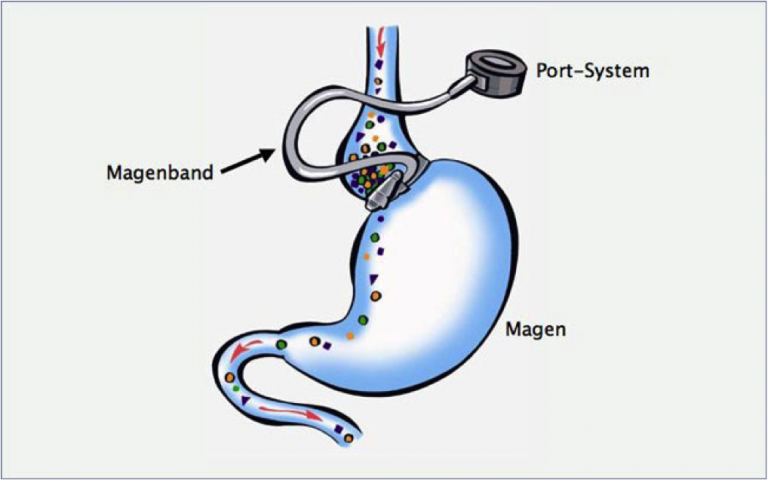
The gastric band is made out of silicone and is placed like a ring around the upper part of the stomach. The stomach band is connected via a tube system with a «reservoir» system that is implanted under the skin. This «reservoir» system can be penetrated with a needle from the outside. By doing so, the gastric band can be adjusted tighter or looser (see sketch).
You can lose an average of 50 % of your excess weight in the long term with a gastric band. However, the quality of life after gastric banding is reportedly lower than after a gastric bypass or a gastric sleeve operation. Weight loss occurs after gastric banding due to the constriction of the stomach by the band, which allows for less food intake.
After gastric binding surgery you are usually hospitalized for 1 – 3 days. The first «adjustment» of the gastric band is done after 6 weeks in conjunction with x-ray checks. Further adjustments are done based on the individual needs of the patient.
The gastric band surgery is a very safe operation with an extremely low complication rate in the first days and months. Some common late complications that have been reported, years after the operation, are the sac-like enlargement of the esophagus (secondary esophagus compensation) and the slippage of the gastric band. Due to these late complications 40 to 50 % of gastric bands have to be removed again.
The gastric band can also be used in addition to the gastric bypass, provided that this is considered a possible and useful treatment after inadequate weight loss following a gastric bypass.
Please visit the bariatric department of the hospital Limmattal during consultation hours for further information on risks and benefits of a gastric band surgery.
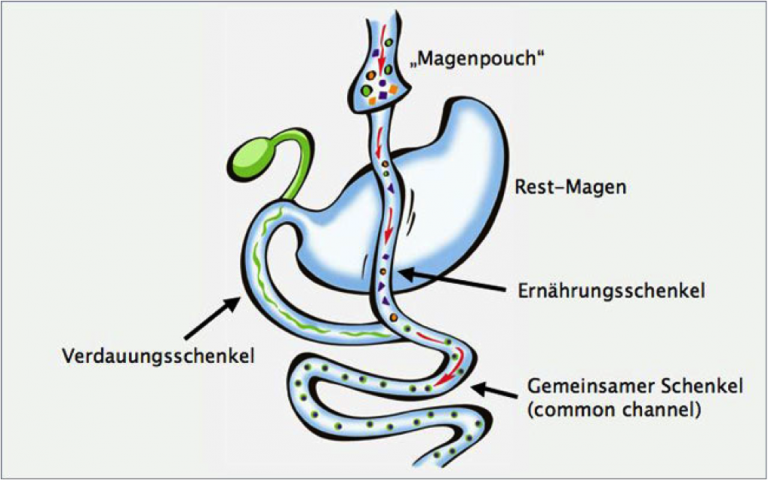
Gastric bypass
(Proximal gastric bypass, distal VVLL gastric bypass, Omega-gastric bypass)
For a gastric bypass, the stomach is cut very high up and connected with a loop of the small intestines that had previously also been cut. Therefore only small meals can be eaten and satiety is reached earlier. The section of the small intestine which carries the digestive juice is reconnected with the food carrying section of the small intestine 2.5 meters (proximal gastric bypass) or 1 meter (distal gastric bypass) before the small intestine connects into the large intestine.
For an Omega gastric bypass only one connection between the stomach pouch and small intestine is established. This results in 2 meters of the small intestine no longer being used as part of the digestion process. The majority of the small intestine is being bypassed reducing the absorption of the energy carriers (fat, sugar, proteins) and, therefore, leading to weight loss.
The gastric bypass has excellent long-term results. Most patients report a good quality of life after a gastric bypass operation.
After a gastric bypass an average of 65 to 70 % of your excess weight can be lost in the long term. In addition, most secondary diseases linked with obesity can be cured or greatly improved (see comorbidities and secondary diseases of obesity).
After a gastric bypass operation you are usually hospitalized for 3 – 7 days. The very rare complications of a gastric bypass (< 0.5 %) in the early phase after the operation (first week) may include secondary bleeding or an anastomotic leak (opening of the mechanical staple seam between the intestines and stomach). The very rare late complications after a stomach bypass include malnutrition and vitamin deficiency symptoms. These possible late complications can be mostly avoided though if you comply with the necessary medical checks, together with blood tests in order to analyse your nutrition status.
Any gap created between the small intestine loops after the gastric bypass is closed by myself immediately so that the risk of internal hernias with intestinal obstruction is below 0.7 %, even years after the gastric bypass operation.
Please visit the bariatric department of the hospital Limmattal during consultation hours for further information on risks and benefits of a gastric bypass operation.
An informative android app can be found at: www.mein-magenbypass.ch
Gastric sleeve

During a sleeve gastrectomy, a thin stomach tube is formed and a large portion of the stomach is removed. In comparison with gastric bypass surgery this procedure has equally good results in weight loss after 5 years. Post operative quality of life is reportedly good. Nowadays gastric sleeve surgery is an established operative method for weight loss.
This operation has been carried out for a shorter period of time in a standardized way than the stomach bypass. As a result no definitive statements can be made for its long-term benefits. The effectiveness of the gastric sleeve (see sketch) is based on the fact that you have to eat smaller portions and the state of satiation is reached earlier. In addition, the gastric sleeve (like the stomach bypass) causes a decrease of appetite hormones, which has a favorable effect on weight reduction.
After a sleeve gastrectomy you are usually hospitalized for 3 – 7 days. The very rare complications after sleeve gastrectomy surgery (approx. 1-2%) may include secondary bleeding in the first 24 hours and the opening of the mechanical staple seam in the stomach during the first 10 days.
Severe malnutrition after a gastric sleeve operation is a rarity (< 0.1 %). Vitamin deficiencies can be avoided if you adhere to the prescribed follow-up medical visits. If the gastric tube does not lead to satisfactory weight loss after several years, it can be converted into a gastric bypass or into a «duodenal switch».
Please visit the bariatric department of the hospital Limmattal during consultation hours for further information on risks and benefits of a sleeve gastrectomy surgery.
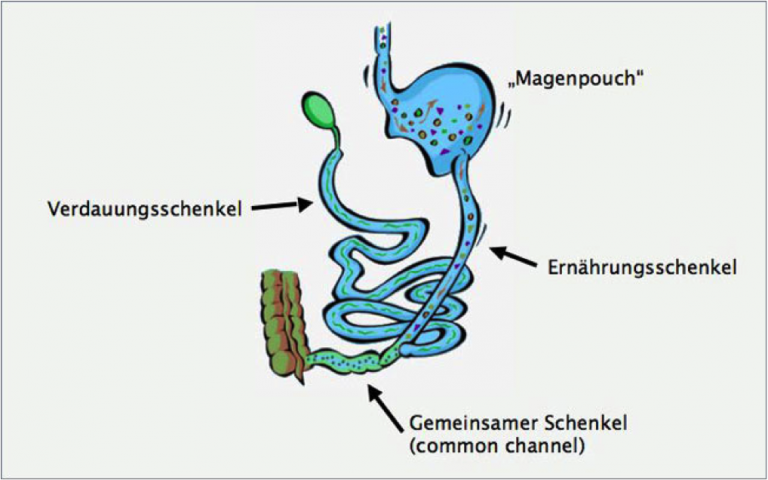
Biliopancreatic diversion
The biliopancreatic diversion can be compared structurally with gastric bypass surgery. In contrast to a gastric bypass however, a much larger part of the small intestine is circumvented from the nutrition system. The resulting weight loss is mainly due to changing the length of the small intestine and therefore less energy carriers (fats, sugars, proteins) have the opportunity to be absorbed from the food into the body.
Biliopancreatic diversion has excellent long-term weight loss results. Most patients report a good quality of life after a biliopancreatic diversion. On average, 75 to 85 % of excess weight can be sustainably lost in the long term with this procedure. In addition, most secondary diseases linked with obesity can be greatly improved or cured.
One disadvantage of the biliopancreatic diversion is the common occurrence of nutrition deficiencies and, therefore, we cannot recommend this operation routinely. However, the surgery is suitable for very severely obese patients (BMI >50) as the first, or second, alternative measure after a gastric bypass or a gastric sleeve, and is possible if the desired results could not be achieved with these initial strategies. Assessment for such an intervention must be made very carefully.
After a biliopancreatic diversion you are usually hospitalized for 5 – 7 days. The very rare complications of a biliopancreatic diversion (<1%) in the early phase after the operation may include secondary bleeding or an anastomotic leak (opening of the mechanical staple seam between intestines and stomach).
The later complications after a biliopancreatic diversion include malnutrition, vitamin deficiency symptoms, anemia, osteoporosis, and gall or kidney stones. In addition, malodorous stools and passing gas may occur often. These possible later complications can be mostly avoided if the patient complies with the necessary medical checks, together with blood tests, in order to analyse nutritional status.
Please visit the bariatric department of the hospital Limmattal during consultation hours for further information on risks and benefits of a biliopancreatic diversion.